Atherosclerosis
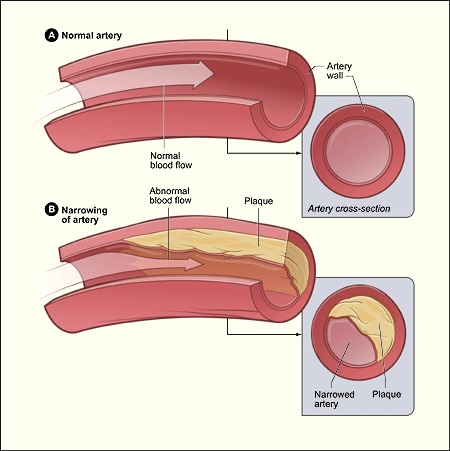
Blood vessels that carry oxygen and nutrients from the heart to the rest of the body are called arteries. Arteries that are not diseased are flexible and elastic. With increasing age and due to other factors, too much pressure in your arteries can make the walls thick and stiff — sometimes restricting blood flow to your organs and tissues. Hardening of arteries ensues which is called as arteriosclerosis. Atherosclerosis is a specific type of arteriosclerosis, but the terms are sometimes used interchangeably. The buildup of fats and cholesterol in and on walls of arteries (plaques) is called as atherosclerosis. This process can restrict blood flow.
Another hazard associated with these plaques is that they can burst, triggering a blood clot. Atherosclerosis is generally considered a problem of arteries of heart, though it can affect arteries anywhere in your body. It is important to recognize that atherosclerosis is a preventable and treatable condition.
9,600+
Happy Patients
10
Qualified Doctors
500+
Successful Surgeries
100+
Insurance Partners
With increasing age, hardening of the arteries occurs. Apart from getting older as a risk factor, other factors that increase the risk of atherosclerosis include:
Atherosclerosis starts in the arteries as early as childhood and is a slow, progressive disease. The precise causes that lead to atherosclerosis are unknown. But, damage or injury to the inner layer of an artery may initiate the process of atherosclerosis. The damage may be caused by:
Damage to the inner arterial walls leads to build up of blood cells and other substances at the injury site and further damaging the inner lining of the artery. With passage of time, fatty deposits (plaques) made of cholesterol and other cellular waste products also build up at the injury site. The hardening and narrowing of your arteries are caused by these plaques. Blocked arteries lead to insufficient blood supply to the organs and tissues connected to themleading improper function of these arteries.
Further, these plaques may break off and enter bloodstream. Additionally, the smooth lining of a plaque may rupture, spilling cholesterol and other substances into your bloodstream. As a result of these changes a blood clot forms which can completely block the blood flow to a specific part of your body. If this happens in arteries of heart, it leads to a heart attack. It is also noteworthy that a blood clot can travel through arteries of other parts of your body and block (partially or totally) blood flow to another organ.
The process of atherosclerosis is a gradual one. Mild atherosclerosis usually doesn’t have any symptoms. The symptoms of atherosclerosis don’t develop until an artery is so narrowed or clogged that it can’t supply adequate blood to your organs and tissues. In extreme circumstances, a blood clot blocks blood flow completely, or even breaks apart and can trigger a heart attack or stroke.
Moderate to severe atherosclerosis can lead to symptoms depending upon which arteries are affected. For example:
If somebody feels he/she has above symptoms pointing towards atherosclerosis, it is important to meet a doctor. One should also be vigilant about early symptoms of inadequate blood flow, such as chest pain (angina), leg pain or numbness. The patients must understand that early diagnosis and treatment can stop atherosclerosis from worsening and prevent a heart attack, stroke or another medical emergency.
During a physical examination, the doctor may find signs of narrowed, enlarged or hardened arteries. These include:
Physical examination signs along with high suspicion could lead to your doctor suggesting one or more diagnostic tests, including:
Location of atherosclerosis determines the complications of atherosclerosis. For example:
The best treatment for atherosclerosis is lifestyle changes that include eating a healthy diet and exercising. But sometimes, medication or surgical procedures may be recommended as well.
Many drugs are available these days that can slow — or sometimes even reverse — the effects of atherosclerosis. Some commonly used drugs are:
More aggressive treatment is required sometimes.Surgical procedures are employed if you have severe symptoms or a blockage that threatens muscle or skin tissue survival. These include:
Lifestyle
Lifestyle changes can help you prevent or slow the progression of atherosclerosis.