Coronary Artery Disease
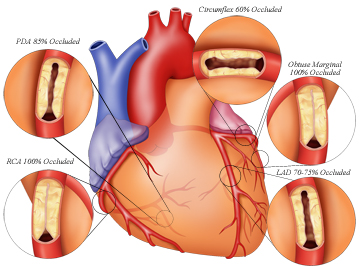
Coronary arteries are the major blood vessels that supply your heart with blood, oxygen and nutrients. Coronary artery disease (CAD) occurs when these arteries become damaged or diseased. The cause mainly is cholesterol-containing deposits (plaque) in your arteries. Narrowing of the arteries occurs when plaques build up, causing your heart to receive less blood. The decreased blood flow, eventually, may cause chest pain (angina), shortness of breath, or other coronary artery disease signs and symptoms. Heart attack occurs when there is a complete blockage.
CAD can go virtually unnoticed until you have a heart attack because coronary artery disease often develops over decades. It can lead to angina or acute myocardial infarction if left untreated. However, one can actually do a lot to prevent and treat coronary artery disease, starting from committing to a healthy lifestyle. Treatment for coronary artery disease can include medications or surgical and minimally invasive procedures.
9,600+
Happy Patients
10
Qualified Doctors
500+
Successful Surgeries
100+
Insurance Partners
There are many risk factors for CAD which includes:
In some cases, CAD develops without any classic risk factors. Researchers are studying other possible factors, including:
Damage or injury to the inner layer of a coronary artery initiates CAD, sometimes as early as childhood. The damage may be caused by various factors, including:
Damage to the inner wall of an artery leads to fatty deposits (plaques) made of cholesterol and other cellular waste products to accumulate at the site of injury in a process called atherosclerosis. Rupture of the surface of these plaques causes blood cells called platelets to clump at the site to try to repair the artery. Heart attack can occur due to this dumping.
Narrowed coronary arteries are unable to supply enough oxygen-rich blood to your heart — especially when it’s beating hard, such as during exercise. Initially, the decreased blood flow may not cause any coronary artery disease symptoms. But, you may develop coronary artery disease symptoms as the plaques continue to build up in your coronary arteries. The symptoms are:
Upon presentation to doctor, a medical history will be taken, a physical exam will be conducted routine blood tests will be ordered. Doctor may suggest one or more diagnostic tests as well, including:
Complications of coronary artery disease are:
Some of the complications of hypertensive retinopathy include:
Treatment of coronary artery disease varies depending on the situation. The patient might be treated with medications, undergo an invasive procedure or both — depending on the severity of the condition and the amount of damage to heart.
Prevention
Effects of PCOS can be offset by paying attention to the foods you eat and your activity levels:
Surgical and other procedures
Additionally, to medications, one of the following procedures might be done to treat your heart attack:
After these medications/procedure, the blood flow to your heart is restored and your condition is stable.
Lifestyle Measures for Prevention
Lifestyle changes can help you prevent or delay the occurrence of heart attack due to coronary artery disease: