Heart Blockage Treatment In Kolhapur
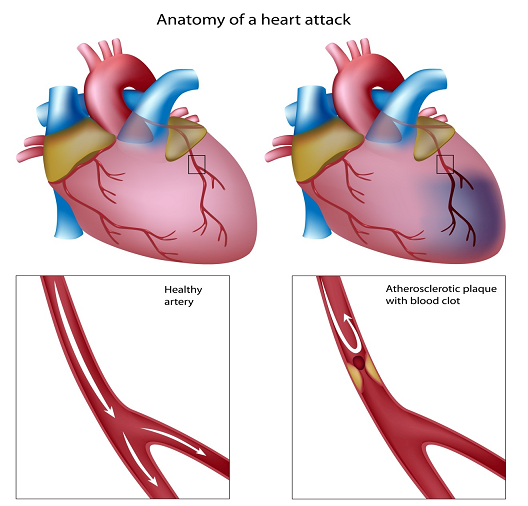
Heart attack, technically known as myocardial infarction (MI) or acute myocardial infarction (AMI), occurs due to the diminution of blood supply to a part of the heart, causing that particular heart cells to die. Heart attack most commonly occurs due to occlusion (blockage) of a coronary artery following the rupture of a vulnerable atherosclerotic plaque. It results in restriction of blood supply and oxygen shortage ensues. If this situation is left as such without treatment for a sufficient period of time, it can cause damage or death (infarction) of heart muscle tissue (myocardium).
A heart attack is a medical emergency. A heart attack usually occurs when a blood clot blocks blood flow to the heart. Without blood, tissue loses oxygen and dies. Symptoms include tightness or pain in the chest, neck, back or arms, as well as fatigue, lightheadedness, abnormal heartbeat and anxiety. Women are more likely to have atypical symptoms than men. Treatment ranges from lifestyle changes and cardiac rehabilitation to medication, stents, and bypass surgery.
9,600+
Happy Patients
10
Qualified Doctors
500+
Successful Surgeries
100+
Insurance Partners
Unwanted buildup of fatty deposits (atherosclerosis) that narrows arteries throughout your body, including arteries to your heart, is contributed by certain factors. It is possible to improve or eliminate many of these risk factors as this decreases your chances of having a first or subsequent heart attack.
Risk factors for heart attack include:
When one or more of the arteries supplying your heart with oxygen-rich blood (coronary arteries) become blocked, it results in heart attack. With passage of time, a coronary artery can become narrowed from the buildup of cholesterol called plaque. This process of plaque of buildup in arteries throughout the body is called atherosclerosis. One of these plaques can rupture during heart attack and a blood clot forms on the site of the rupture. A complete blockage of flow through artery occurs if the clot is large enough. Coronary artery disease occurs when your coronary arteries have narrowed due to atherosclerosis. Most heart attacks occur due to coronary artery disease.
Spasm of a coronary artery that shuts down blood flow to part of the heart muscle is another uncommon cause of a heart attack. Life-threatening spasm can occur due to drugs such as cocaine. A tear in the heart artery (coronary artery dissection) can also cause heart attack. Small blood clots or tumors that have traveled from other parts of the body (coronary embolism) are other uncommon causes of heart attack.
The heart attack is culmination of a several hours long process. More heart tissue is deprived of blood and deteriorates or dies with each passing minute. Damage to the heart can be limited or prevented if blood flow can be restored in time.
Most common symptoms of heart attack are:
Women patients have different or atypical signs and symptoms of heart attack, which include:
Symptoms of heart attack may vary. All patients of heart attack do not experience the same symptoms or experience them to the same degree. Another interesting feature is that many heart attacks aren’t as dramatic as the ones you’ve seen on TV. In some patients, there are no symptoms at all. Still, the more signs and symptoms you have, the greater the likelihood that you may be having a heart attack.
The timing of heart attack is not fixed and it can occur at any time of the day— at work or play, while you’re resting, or while you’re in motion. In some patients heart attacks strike suddenly, but many people who experience a heart attack have warning signs and symptoms hours, days or weeks in advance. Most common and earliest warning of a heart attack may be recurrent chest pain (angina) that are triggered by exertion and relieved by rest. A temporary decrease in blood flow to the heart causes angina.
If a patient is having a heart attack or is suspecting having one, his/her diagnosis will likely happen in an emergency setting. You will be undergoing certain tests that will help check if your signs and symptoms, such as chest pain, signal a heart attack or another condition. These tests include:
Additional tests
After taking immediate steps to treat your condition, doctor may order for these additional tests:
Complications of heart attack are often related to the damage done to your heart during a heart attack. Most common problems arising due to damage to heart are:
Treatment of a heart attack varies depending on the situation. The patient might be treated with medications, undergo an invasive procedure or both — depending on the severity of the condition and the amount of damage to the heart.
More heart tissue loses oxygen and deteriorates or dies with each passing minute after a heart attack. Restoration of blood flow quickly is the main way to prevent heart damage. Medications given to treat a heart attack include:
Surgical and other procedures
Additionally, to medications, one of the following procedures might be done to treat your heart attack:
After these medications/procedure, the blood flow to your heart is restored and your condition is stable following your heart attack. You may be kept in the hospital for observation.
Lifestyle Measures for Prevention
Lifestyle changes can help you prevent or delay the occurrence of heart attack.